Editor’s Note: This paper is published as part of the Hutchins Center on Fiscal and Monetary Policy’s Productivity Measurement Initiative in partnership with the USC-Brookings Schaeffer Initiative for Health Policy, which is a partnership between Economic Studies at Brookings and the University of Southern California Schaeffer Center for Health Policy & Economics.
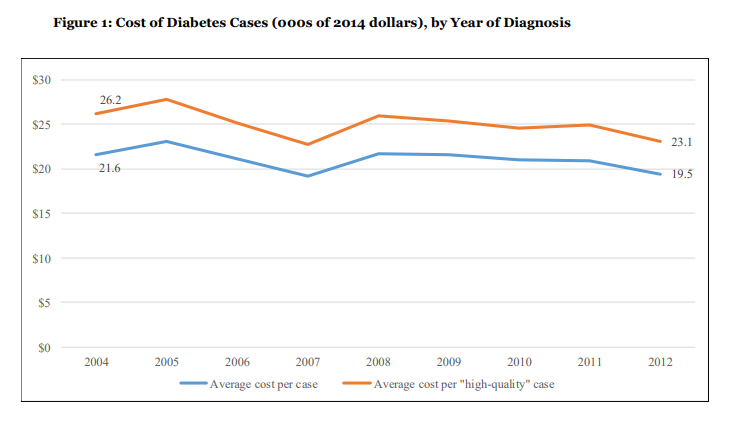
Recent assessments of acute episodes of care point to productivity growth stemming from improvements in patient outcomes. This study assesses productivity growth in the treatment of a major chronic condition, specifically, type 2 diabetes. Analyzing traditional Medicare beneficiaries with new diagnoses over 2004-2012, the authors find that the productivity of health care improved at an annualized rate of 2.2 percent. In this context productivity growth translated into only modest improvement in patient outcomes; most of the growth was realized in the form of lower treatment costs.
To the authors’ knowledge, this is the first study that assesses productivity growth among health care providers in treating a major chronic condition. Nevertheless, it is important to recognize that compelling evidence exists with respect to the social value of evolving treatments for chronic diseases, and to place the current findings in that broader context. The productivity improvement found in this study manifested itself partly in the form of better health outcomes, but mainly as a substantial decline in treatment costs. Specifically, costs decreased in the base analysis by 11.5 percent over 2004-2012, for an annualized rate of 1.3 percent. By contrast, recent studies of the delivery of acute care have found flat-to-increasing costs, with productivity improvement manifested in the form of improved outcomes for patients.
The focus in the current study on a representative sample of individuals with an important chronic condition and coverage from a large national insurance program promises some generalizability of our findings to other contexts. Even so, there is clearly a critical need and opportunity to deepen our understanding of productivity in health care delivery. A worthwhile next step would be to explore how the use of primary and other types of health care have evolved among patients with early as well as advanced diabetes.