Abstract
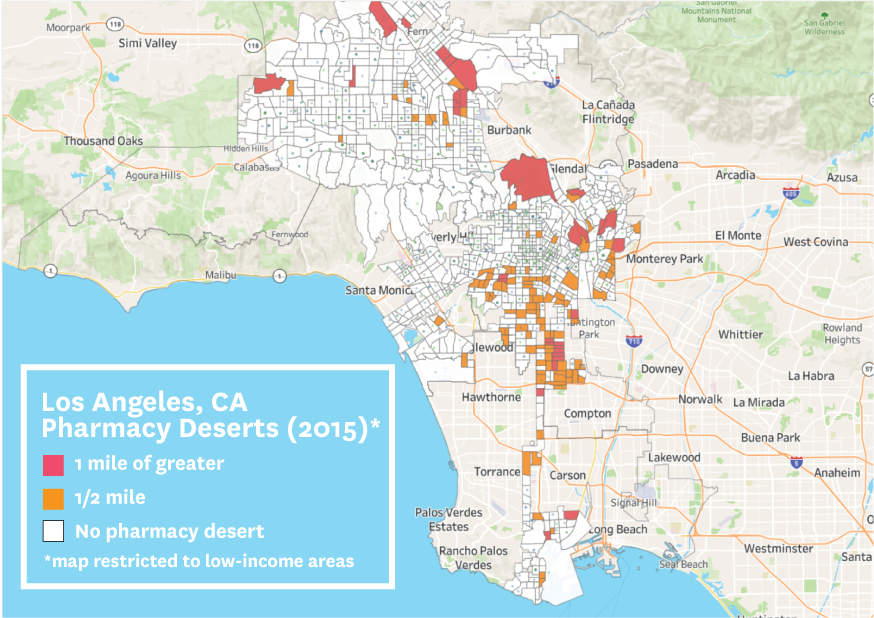
The accessibility of pharmacies may be an overlooked contributor to persistent racial and ethnic disparities in the use of prescription medications and essential health care services within urban areas in the US. We examined the availability and geographic accessibility of pharmacies across neighborhoods based on their racial/ethnic composition in the thirty most populous US cities. In all cities examined, we found persistently fewer pharmacies located in Black and Hispanic/Latino neighborhoods than White or diverse neighborhoods throughout 2007–15. In 2015 there were disproportionately more pharmacy deserts in Black or Hispanic/Latino neighborhoods than in White or diverse neighborhoods, including those that are not federally designated Medically Underserved Areas. These disparities were most pronounced in Chicago, Illinois; Los Angeles, California; Baltimore, Maryland; Philadelphia, Pennsylvania; Milwaukee, Wisconsin; Dallas, Texas; Boston, Massachusetts; and Albuquerque, New Mexico. We also found that Black and Hispanic/Latino neighborhoods were more likely to experience pharmacy closures compared with other neighborhoods. Our findings suggest that efforts to increase access to medications and essential health care services, including in response to COVID-19, should consider policies that ensure equitable pharmacy accessibility across neighborhoods in US cities. Such efforts could include policies that encourage pharmacies to locate in pharmacy deserts, including increases to Medicaid and Medicare reimbursement rates for pharmacies most at risk for closure.
Pharmacies are an increasingly important point of care for neighborhoods in the US. They not only dispense prescription medications but also offer diagnostic, preventive, and emergency services, including in response to the COVID-19 pandemic. Despite the critical role of pharmacies in facilitating access to prescription medications and essential health care services, however, there is limited information on disparities in the availability and geographic accessibility of pharmacies in urban areas.
Prior studies have examined the availability of pharmacies at the county level and report that although urban areas have a greater number of pharmacies than their rural counterparts, pharmacies located in urban areas are more likely to experience closures—particularly independent stores serving low-income, minority populations. Pharmacies located in urban areas are also less likely to meet Centers for Medicare and Medicaid Services convenient access standards when compared with suburban and rural pharmacies.
In a 2014 report we found that pharmacy deserts, defined as neighborhoods with low geographic access to pharmacies, are disproportionately more prevalent in segregated Black and Hispanic/Latino neighborhoods in Chicago, Illinois. Many of these neighborhoods have also experienced recent waves of pharmacy closures, which worsened during the COVID-19 pandemic and the civil unrest in June 2020. Therefore, residents of Black and Hispanic/Latino neighborhoods, who already have lower rates of medication adherence, need to travel even farther to their nearest pharmacy to obtain their prescription medications.
Closures and the resulting pharmacy deserts are expected to increase because of the growth of pharmacy benefit managers, which contribute to lower reimbursement rates to pharmacies.13 Although many rural states provide higher Medicaid reimbursement rates for pharmacies at risk for closure, similar policies have not been implemented in urban areas. In July 2018 Illinois became the first state to implement a Critical Access Pharmacy payment policy that would provide higher reimbursement rates for Medicaid prescriptions dispensed at independent pharmacies located in both urban and rural Medically Underserved Areas.
The goal of this study was to examine whether the availability and geographic accessibility of pharmacies varied by neighborhood racial/ethnic composition in the thirty most populous cities in the US. We focused on disparities in the accessibility of pharmacies in cities because more than 80 percent of the Black and Hispanic/Latino populations in the US live in cities, and there is evidence that the accessibility of pharmacies contributes to racial/ethnic disparities in adherence to prescription medications. We hypothesized that segregated Black and Hispanic/Latino neighborhoods in all cities had fewer pharmacies and were more likely to be pharmacy deserts than other neighborhoods in these cities.
We also examined whether pharmacy deserts were more prevalent in Medically Underserved Areas because several federal and state policies attempting to address barriers in accessing pharmacies and medications, including the 340B Drug Pricing Program and the Illinois Critical Access Pharmacy program, target Medically Underserved Areas. As a consequence, our findings can inform policy efforts to better ensure equitable access to pharmacies in urban areas, as well as to the medications and services they provide.
A press release about the study is available here. The full study is available here.