A More Resilient, Affordable Healthcare System
As healthcare spending approaches 20% of gross domestic product, the pressure to “bend the cost curve” has never been stronger. Many have argued that the answer is to just lower prices by government fiat.
However, the right policies need to focus on the price of health, not healthcare. This is especially true for diseases with few or no treatment options. The least affordable drugs and technologies are those that haven’t been discovered. Just think about how much society was willing to pay for an effective COVID-19 vaccine.
At the Schaeffer Center, we’ve spent over a decade conducting evidence-based research to ensure access to high-value healthcare, build a healthcare system that is resilient and sustainable, and encourage biomedical innovation that improves quality of life.
Cancer provides a poignant example. Our experts have developed pricing models to reward high-value advances while protecting against paying for treatments that don’t work. We’ve also shown that outcomes improve significantly—and disparities can be reduced—when the disease is caught early. Yet not everyone receives recommended routine screenings, which contributes to racial and ethnic disparities in cancer survival rates. Schaeffer Center research found that blood-based tests that can detect multiple cancers could be a critical tool in addressing these challenges.
Passing savings on to consumers can improve adherence and access to medications, but complicated, opaque payment systems do not always result in lower costs for patients. Over the past year, our researchers illuminated the role of intermediaries in the pharmaceutical supply chain.
We were thrilled to see policymakers take note of this work as they develop solutions to address the high and rising drug costs consumers are shouldering. Of course, lower drug prices mean little to underserved areas that lack pharmacies in the first place. Groundbreaking Schaeffer Center work highlights the issue of pharmacy deserts—an often-overlooked factor in healthcare disparities.
An affordable healthcare system necessitates evaluating the full cost—not just the cost borne by the patient. Through the leadership of the USC-Brookings Schaeffer Initiative for Health Policy, the federal No Surprises Act—which eliminates the practice of surprise medical billing—shields patients from excessive billing for out-of-network services while simultaneously containing costs for healthcare providers and payers.
Our scholars collaborate across disciplines to conduct research aimed at improving value in health. This year we welcomed Richard Frank as the new director of the USC-Brookings Schaeffer Initiative for Health Policy. He succeeds Paul Ginsburg, who continues as a Schaeffer Center senior fellow—and whose exemplary leadership in health policy resulted in his election to the National Academy of Medicine. We also welcomed Matthew Kahn, provost professor of economics at the USC Dornsife College of Letters, Arts and Sciences, who will lead our newest research program—the Healthcare Markets Initiative.
As always, we remain grateful to Leonard Schaeffer and his wife, Pamela, our Advisory Board, and the partnership of USC’s Price School of Public Policy and School of Pharmacy. Their support and the excellence of our fellows ensure that the Schaeffer Center will always be a beacon in guiding policymakers and the public toward an affordable, sustainable healthcare system.
Dana Goldman
Erin Trish
Co-Directors, USC Schaeffer Center


Explore Schaeffer Center Research ↓

- Before policymakers attempt to address rising prescription drug costs, they need to follow the money. As drug spending rises, so do calls to rein in costs—but some responses risk stunting the medical discoveries essential to saving and improving lives. The Schaeffer Center works to shine a spotlight on the big picture to better inform pricing and reimbursement policies.
-
Policymakers and the media tend to focus on manufacturers when discussing the costs of prescription drugs, with little attention paid to the middlemen—wholesalers, pharmacy benefit managers (PBMs), pharmacies and insurance companies—who also add costs but contribute little innovation. Major Schaeffer Center studies in 2021 investigated these and other aspects of the pharmaceutical distribution system to reveal the rewards to different distribution system players.
The Schaeffer Center Value of Life Sciences Innovation program provides evidence-based strategies to enhance cost-effective healthcare delivery while ensuring a healthy ecosystem for ongoing innovation.
Promoting Competition in the Supply Chain
Improving value and expanding access to care requires uncovering where savings can be achieved. To determine whether some players are earning excessive profits relative to the risk they bear, Neeraj Sood, Karen Mulligan and Kimberly Zhong factored in financial risk to calculate the investment returns for manufacturers and middlemen in the pharmaceutical supply chain.
After accounting for research and development, the authors showed that risk-adjusted returns were actually lower for pharmaceutical manufacturers compared to the Standard and Poor’s 500 index (1.7% vs. 3.6%). However, risk-adjusted returns for biotech manufacturers (9.6%), wholesalers (8.1%) and insurers/PBM/retailers (5.9%) outpaced the S&P 500 from 2013–2018, according to the study.
Revealing the Role of Middlemen
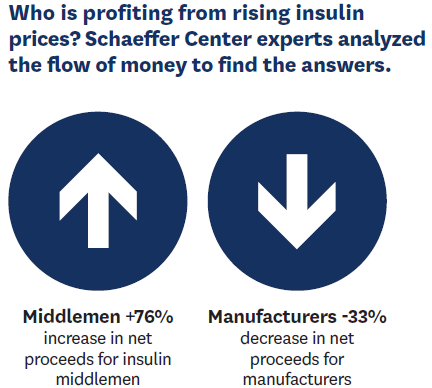
The question of who is benefiting from rising insulin prices remained a mystery until Schaeffer Center experts analyzed distribution complexities to find answers—offering one of the most comprehensive looks at the insulin distribution system. In research published in JAMA Health Forum, Karen Van Nuys, Neeraj Sood and Rocio Ribero analyzed the money flow across the web of insulin manufacturers, wholesalers, pharmacies, PBMs and health plans.
The team found that, while the total expenditures per unit of insulin remained relatively flat between 2014 and 2018, middlemen in the distribution system collected nearly 53% of the net proceeds from insulin sales in 2018—up from 30% in 2014. Meanwhile the share going to manufacturers decreased by 33%.
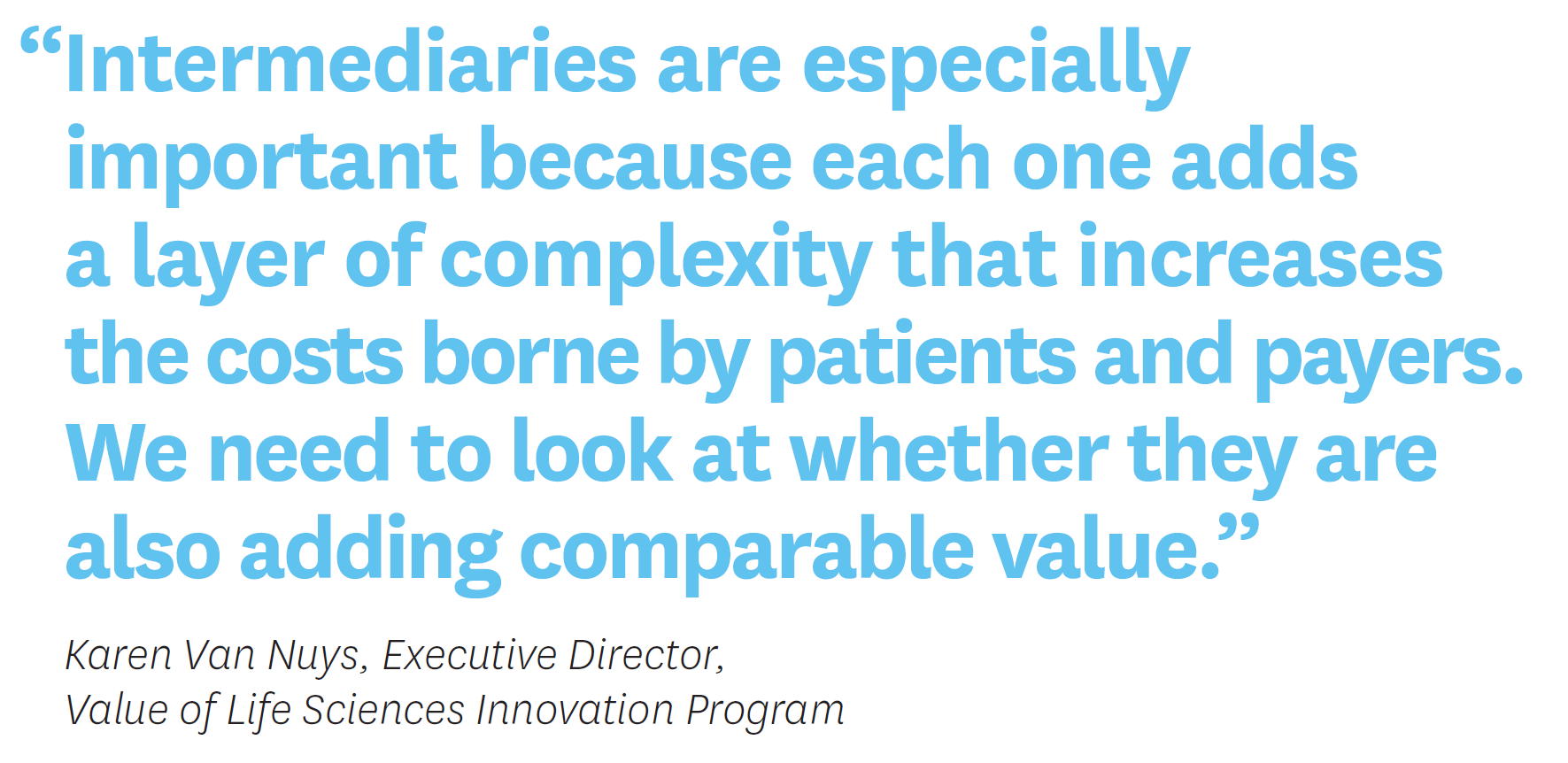
While manufacturers are accepting lower prices, patients are not seeing the benefit of this decrease. “Policymakers should bring together all players in the distribution system, require a transparent accounting of financial flows at each step, and from there develop solutions that improve health and systemwide affordability,” Van Nuys says.
“Clearly all entities in the pharmaceutical distribution system profit from the sale of insulin,” Sood notes. “But these data suggest that increasing profits to intermediaries in the system are playing a key role in keeping net expenditures high.”

Karen Van Nuys, Executive Director, Value of Life Sciences Innovation Program. Passing on Savings to Consumers
Market efficiency is crucial to cost-effectiveness. For research published in JAMA Internal Medicine, Erin Trish, Karen Van Nuys, Rocio Ribero and Geoffrey Joyce examined what Medicare Part D plans paid for the most commonly prescribed generic drugs compared to the cash prices available to Costco members for the same prescriptions in 2017 and 2018. Across more than 1.4 billion Part D claims for 184 products, they found that Medicare plans overspent by 13% in 2017 and almost 21% in 2018, compared to Costco. These overpayments amounted to $2.6 billion in 2018 alone.
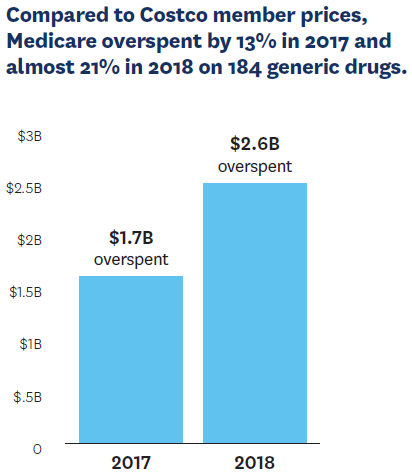
Medicare Part D is administered through private plans that negotiate via PBMs on behalf of the Medicare system. While PBMs are large, sophisticated agents that can negotiate low prices from competing manufacturers, the problem, according to the research, is that PBMs and other intermediaries in the system are not passing the savings from the negotiated prices to the plans and the patients.
“Our analysis shows that, in systems Like Costco’s, where incentives are set up to deliver value directly to the consumer at the pharmacy counter, that’s what happens,” Trish says. “It’s time to fix those incentives in the Medicare Part D system to put the patient first.”
The study—which found $2.6 billion in 2018 overpayments on just 184 drugs—also shows that more attention should be paid to generic prices and not just brand-name drug costs. “Efforts to reduce prescription drug prices tend to focus on brand-name medicines, but the opaque pharmaceutical supply system can also cause health plans and taxpayers to overpay for generics,” Joyce notes.
Reducing Disparities in Cancer Detection
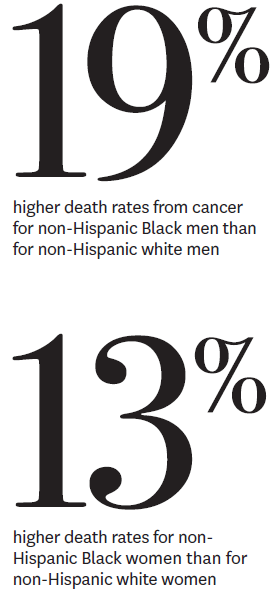
Early cancer detection is crucial to enhancing patient survival rates, yet economic obstacles and cultural attitudes can keep Black and Latino patients from undergoing recommended screenings. A study by Alison Sexton Ward, Karen Van Nuys and Darius Lakdawalla addressed the benefits of multi cancer blood-based tests—which do not require a specialist to administer them—while also examining the factors driving disparities.
Insufficient insurance coverage and a lack of trust in healthcare providers that can stem from the disproportionately lower-quality facilities that serve many minority communities are among the factors driving disparities in health outcomes.
“The promise of these tests will only be realized if we are able to provide broad access to vulnerable populations,” Lakdawalla says.

- “The start of the pandemic occurred while we saw fentanyl infiltrating the West Coast. We find this challenging confluence of events— including the stay-at-home orders— impacted opioid-related behaviors differently across communities.”
– Jason Doctor, Co-Director, Behavioral Sciences Program -
Behavioral science blends insights from psychology, economics and other social sciences to understand how people make decisions. The Schaeffer Center applies the field’s knowledge to find ways to improve health, including understanding decision-making surrounding COVID-19 and opioid use.
Locking Down Opioid Fatalities
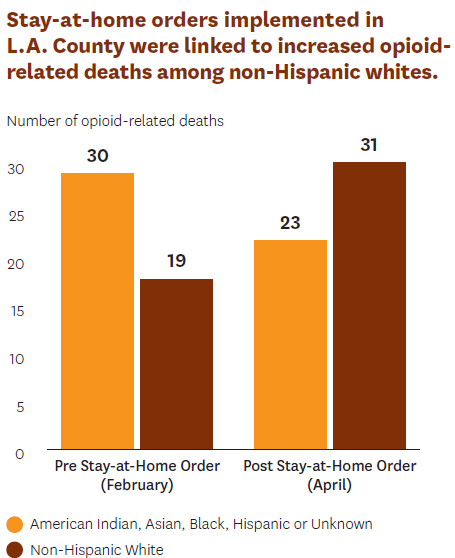
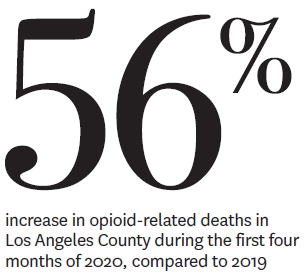
Early in the pandemic, many cities swiftly enacted stay-at-home orders for public safety, but these policies also had tragic side effects for some populations. Jason Doctor led research investigating the impact of lockdown orders on fatal opioid overdoses. The study, published in Drug and Alcohol Dependence, found that stay-at-home directives implemented during March and April 2020 were associated with increased opioid-related deaths among white populations, while such fatalities decreased among Black, Asian and Hispanic populations.
“The start of the pandemic occurred while we saw fentanyl infiltrating the West Coast,” Doctor says. “We find this challenging confluence of events—including the stay-at-home orders impacted opioid-related behaviors differently across communities.”
The people who died were mostly white males residing in areas where a smaller share of the adult population has a bachelor’s degree. The decrease in face-to-face treatment options that followed the orders may have contributed to this increase in overdoses, Doctor says. Further, while the research was limited to Los Angeles, its findings mirror troubling trends among middle-aged white Americans across the country who live in areas where few people hold bachelor’s degrees.
Promoting Protective Behaviors
The COVID-19 pandemic has forced us to learn new protective behaviors against infectious disease. But whether individuals adopt these measures may depend in part on how they associate COVID-19 with other infectious diseases.
Wändi Bruine de Bruin led a study, published in Social Science & Medicine, that asked 6,534 U.S. adults to list conditions that came to mind when they thought of COVID-19. Participants also completed questions that asked about demographics, risk perceptions and protective behaviors. Seasonal influenza (59%) was the most common illness mentioned across all demographic groups, followed by pandemic influenza (28%), SARS/MERS (27%), Ebola (14%), common cold (11%) and pneumonia (10%).
With few exceptions, mentions of seasonal influenza or the common cold tended to be associated with a lower likelihood of self-reported protective measures: 55% of individuals who associated COVID-19 with seasonal flu and 51% of those who associated it with the common cold reported that they were avoiding crowds as a protective behavior. In comparison, 62% of people associating COVID-19 with pneumonia said they were actively avoiding crowds.

The findings suggest that public health communicators need to recognize the potential impact of infectious disease comparisons on public behavior—and focus on what protective behaviors are most needed in the particular situation.
Communicating well about any topic—from COVID-19 to climate change—requires understanding the audience. Bruine de Bruin is an expert in risk communication and is working to expand this research to encompass a more global community. With funding from the Lloyd’s Register Foundation, she will use insights from the World Risk Poll report to help international organizations make their risk messages more effective.
Understanding Physician Decision-Making
Clinicians frequently over-order tests and treatments that are not in line with prevailing recommendations. This is especially the case when caring for older patient populations. Jason Doctor and colleagues published a study to understand why physicians order these potentially unnecessary tests.
The team found that physicians are aware and knowledgeable of the testing guidelines, but many deferred to patient preference when deciding whether to order a test. Furthermore, clinicians tended to overestimate the benefits of testing and underestimate the harms or downsides. Policymakers and stakeholders interested in decreasing unnecessary testing and treatment in older adults should take these findings into account. This study builds on a body of work by Doctor and colleagues to improve physician decision-making and patient health outcomes.

Jason Doctor and Wändi Bruine de Bruin, Co-Directors, Behavioral Sciences Program.

- Despite efforts to end the opioid crisis, some communities suffered more deaths in 2020 than ever before. From combating the opioid crisis to eliminating pharmacy deserts, improving health starts at the community level. Schaeffer Center researchers are analyzing the impact of cannabis regulation, pharmacy closures and addiction treatment options that were available during the pandemic to devise better approaches to improve population health.
-

Reducing Opioid Overdose Risk
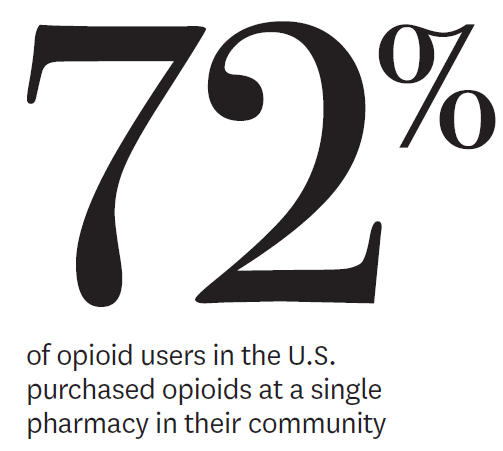
While public awareness and efforts to stop addiction and overdoses have intensified, some communities reported higher rates of opioid-related deaths in 2020 than ever before. Recent research led by Dima M. Qato reveals that, although high-risk prescription opioid use has declined, nearly 1 in 10 adults takes opioids that put them at increased risk of an overdose.
“These findings underscore the importance of strengthening the implementation of overdose prevention, particularly naloxone access laws, and harm-reduction strategies,” Qato says.
Qato and colleagues examined a representative, 5% sample of anonymized data drawn from individual prescription claims from 2011 though 2016. The study analyzed use among U.S. adults age 18 and older who filled prescriptions at retail pharmacies.
The research team factored in dangerous co-prescriptions of benzodiazepines, a class of sedatives commonly prescribed for anxiety, seizures or insomnia. Combining opioids with benzodiazepines further increases the risk of overdose and death, the investigators found. More than half of high-risk prescription opioid users received their prescriptions from a single provider. The study detected higher rates of risk among older consumers, who tended to use Medicare for payment. They were also more likely than their younger counterparts to have multiple prescribers and purchase from multiple pharmacies.
The pandemic, however, may have positively impacted treatment options for individuals with opioid addictions. While these patients have long relied on in-person individual therapy or group support for sustained recovery, such activities became too dangerous in the early days of the pandemic. Rosalie Liccardo Pacula and her colleagues analyzed state and federal responses to the opioid crisis amid the pandemic and found that, while all states and the District of Columbia adopted at least one policy related to treatment access for patients suffering from opioid addiction, no states adopted all policies important to treatment access.

Capping Cannabis Potency
Even as states rush to legalize cannabis, much work remains for public health regulation— especially since the federal government has shied away from issuing nationwide safety standards. One concern is that most states base sales limits on a product’s weight instead of the tetrahydrocannabinol (THC) levels that determine potency.
Research by Rosalie Liccardo Pacula reveals that, although wide variation exists in the total grams of THC that can be purchased at once, all states allow sales of 500 doses or more of 10 milligrams per transaction. Such a quantity can supply a typical user for at least a month. Pacula’s analysis, published in the American Journal of Preventive Medicine, suggests the need for stricter caps.
“Sales limits are usually put in place to encourage moderation and to prevent diversion from the legal to the illegal market,” Pacula notes. “The limits applied by U.S. states today will not accomplish either of these objectives.”
Improving Screening of Minors
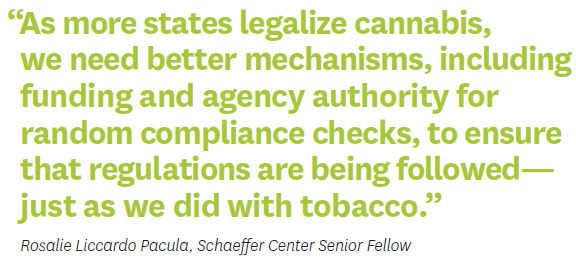
Even though California forbids cannabis dispensaries from selling to minors, a study co-authored by Rosalie Liccardo Pacula reveals the ineffectiveness of these restrictions. Published in JAMA Pediatrics, the project sent young researchers to 700 licensed dispensaries across the state to test their screening processes. The field researchers assessed the use of such measures as age-limit signage and ID checkpoints. They also considered the presence of marketing materials that could appeal to children.
Although 97% of the dispensaries employed ID checks, only 12% did so before buyers entered the store. In addition, nearly 68% failed to comply with age-limit signage, and 35% also sold items that could appeal to children and teens.
As more states lift restrictions on recreational cannabis, Pacula recommends mandated random compliance checks and financial penalties for delinquencies. Just as tobacco sales fund checks of cigarette sellers, cannabis companies could support better policing of their dispensaries.

Eliminating Pharmacy Deserts
Pharmacies are an increasingly important point of care for neighborhoods in the U.S. They not only dispense prescription medications but also offer diagnostic, preventive and emergency services. Lack of access to a convenient pharmacy may be an overlooked contributor to persistent racial and ethnic disparities in the use of prescription medications and essential healthcare services within urban areas in the U.S.
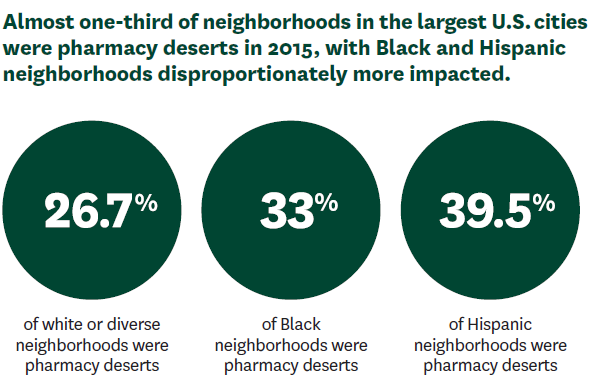
A study by Dima M. Qato and colleagues demonstrated that Black and Latino neighborhoods in the 30 most populous U.S. cities had fewer pharmacies than white or diverse neighborhoods between 2007–2015. The team also found that Black and Latino neighborhoods were more likely to experience pharmacy closures compared with other neighborhoods. Qato coined the term pharmacy desert to describe areas where residents cannot fill a prescription within one mile, or half a mile for low-income residents without a vehicle.
“Our findings suggest that addressing disparities in geographic access to pharmacies—including pharmacy closures—is imperative to improving access to essential medications and other healthcare services in segregated minority neighborhoods,” Qato says.
These efforts could include policies that encourage pharmacies to locate in pharmacy deserts, such as increases to Medicaid and Medicare reimbursement rates for pharmacies most at risk for closure.

- “Alzheimer’s disease will impose a significant burden on society in the coming decades. It’s imperative we identify ways to accelerate the clinical pipeline to change the trajectory.”
– Julie Zissimopoulos, Co-Director, Aging and Cognition Program -
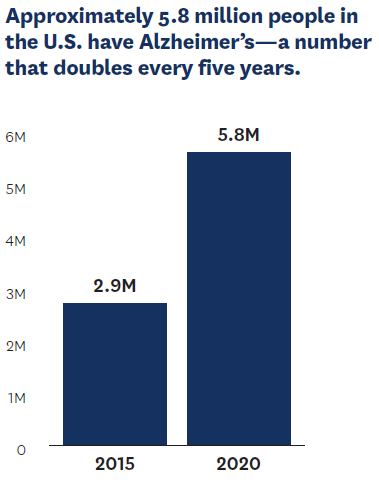
While the healthcare profession has achieved remarkable progress in lengthening life expectancy, more must be done to ensure that those added years are healthier ones. Longer lifespans have led to an explosion in rates of Alzheimer’s and other age-related disorders. Approximately 5.8 million people in the U.S. alone have the ultimately fatal condition of Alzheimer’s—a number that doubles every five years among those older than 65. However, better therapies are being developed, and the Schaeffer Center is at the forefront of devising strategies to expedite the availability of future breakthroughs to reach everyone who can benefit.
Breaking Down Barriers
Randomized clinical trials are essential to the drug-approval process, but people with Alzheimer’s disease face numerous obstacles to accessing them. With support from Gates Ventures, Schaeffer Center investigators surveyed nearly 900 clinical trial personnel, patients, caregivers and physicians to better understand these hurdles and develop strategies for overcoming them.
The challenges identified include limited physician and patient awareness of the early stages of Alzheimer’s, fear of diagnosis, overstretched healthcare systems and a shortage of fast yet inexpensive diagnostics. These barriers result in approximately 99% of potential participants either not considering or never being referred to a clinical trial.
Advancing Social Science Research
Unless cures are found, the cost of caring for patients with Alzheimer’s disease and related dementias (ADRD) is projected to reach $1.5 trillion by 2050. Solutions are needed to improve care, support caregivers and quantify the impact of these trends.
Julie Zissimopoulos has been helping lead the national conversation. She co-directs the National Institutes of Health–funded Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and the Alzheimer’s Disease Resource Center for Minority Aging Research. In addition, she was nominated to co-chair the 2022 ADRD Summit Health Equity Sub-Committee. As a member of the National Academies of Sciences, Engineering and Medicine’s Committee on Developing a Behavioral and Social Science Research Agenda on Alzheimer’s Disease, she produced a report outlining a 10-year research agenda in the behavioral and social sciences as it relates to ADRD.
“Much of the current research into ADRD is focused within biology, biochemistry and pharmaceutical innovation,” Zissimopoulos says. “But we know Alzheimer’s is also a social disease with devastating socioeconomic impacts. The social sciences have an important role to play in understanding and developing solutions to the burden of ADRD.”
This work complements USC’s vast achievements in Alzheimer’s research, which include mapping its spread in the brain, developing the first regenerative therapy to be tested for the disease and discovering how leaky blood vessels can indicate early onset.
Delivering Palliative Care Optimally
With a focus on improving quality of life and reducing the burden on seriously ill patients and their families, palliative care—provided alongside other therapy—is used to treat pain and other distressing symptoms, address family needs, coordinate care, and offer emotional and spiritual support.
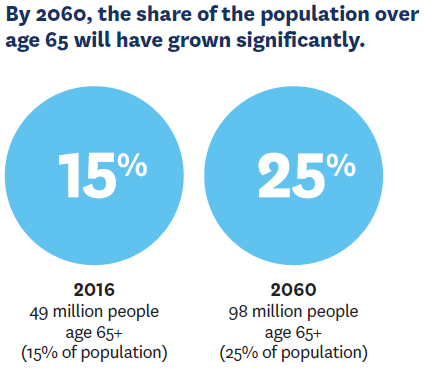
By 2034, more people in the country will be age 65 and older—the group at highest risk for cancer and other serious illness—than under 18. With our aging society, effective palliative care is increasingly vital. But palliative care teams of specialists, nurses, social workers and chaplains are rarely used. Mireille Jacobson, Bryan Tysinger and colleagues participated on a Schaeffer Center advisory committee to develop a research agenda aimed at identifying evidence-based solutions to expand access to such care.
In an op-ed for STAT, Jacobson and R. Sean Morrison, a geriatric and palliative medicine physician at Mount Sinai Health System, wrote: “Over the course of their lives, most people will develop one or more serious illnesses they will live with for many years. We have a treatment—palliative care—that can increase quality of life and longevity. It’s past time to take the necessary steps to ensure that everyone has access to it.”

Mireille Jacobson and Julie Zissimopoulos, Co-Directors, Aging and Cognition Program.

- COVID-19 has had tragic consequences for the elderly—but no one is immune. Our research reveals the pandemic’s hidden costs. From the pandemic’s earliest days, Schaeffer Center experts have armed policymakers at all levels with the research-driven insights essential to improve access to care and reduce the burden of COVID-19.
-
Uncovering COVID’s Overlooked Toll
At first glance, statistics appear to support the common perception that COVID-19 does its worst damage among the elderly and vulnerable. But these grim numbers mask another reality—and focusing on them has biased policy decisions and individual choices.
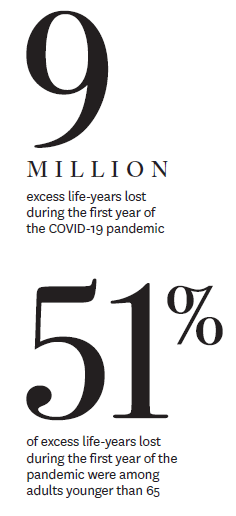
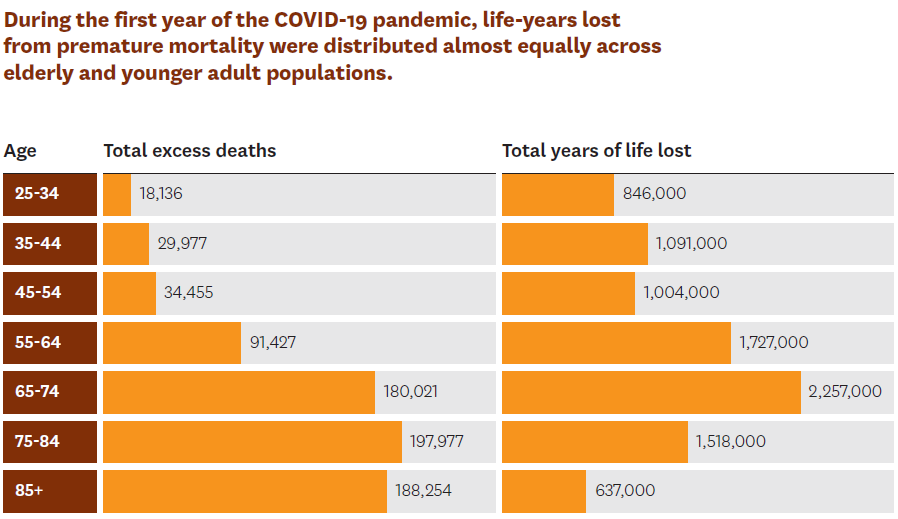
Schaeffer Center researchers found that elderly and younger adult populations have borne a significant burden from the pandemic when measured by years of life lost. In total, over 9 million years of life were lost in the first year of the pandemic, with adults ages 25 to 64 accounting for 51% of these lost birthdays.
The analysis leveraged the Schaeffer Center’s Future Elderly Model and Future Adult Model and was published in Annals of Internal Medicine.
“The focus on older people passing away from COVID misses the substantial burden COVID has imposed on younger people with chronic conditions like obesity,” Darius Lakdawalla says. “Many people have emphasized that protections like lockdowns and vaccinations ought to focus on the old and the vulnerable. However, our findings contradict the belief that this is a pandemic primarily of the elderly.”
Neeraj Sood is evaluating the impact of stay-at-home orders and other policy interventions aimed at stopping the spread of the virus. Published as a National Bureau of Economic Research working paper, his research finds that stay-at-home orders may have caused additional unintended harms and been largely ineffective in the U.S. in reducing excess mortality.
Understanding Disparities in Vaccination Rates
John Romley and Matthew Crane assessed the relationship between county COVID-19 vaccination rates and both social vulnerability and vaccine hesitancy to understand the link between these interconnected issues and vaccination uptake.

They found that nearly 20% of counties are associated with high levels of both hesitancy and social vulnerability and continue to be most at risk of failing to achieve high vaccination coverage. Furthermore, their analysis, published in Health Affairs, showed vaccine hesitancy and social vulnerability have independently impacted vaccine rates—an important finding for policymakers.
By early August, counties with high hesitancy had an average vaccination rate 17% lower than counties with low hesitancy, even after adjusting for the Center for Disease Control and Prevention’s social vulnerability index (SVI).
Meanwhile, disparities between counties with moderate to low SVI and high SVI were relatively smaller but have widened substantially. The coverage difference between low-and high-SVI counties increased from 1.8% in March 2021 to 4.6% in August 2021.
The way vaccines were initially allocated may also play a role in uptake, according to research by behavioral scientist Wändi Bruine de Bruin. She and Dana Goldman found that allocation practices may contribute to vaccine-hesitant individuals later refusing the shot when it is made available to them.
“Disinterest in getting the vaccine increased among all groups when they were overlooked and had to wait,” Bruine de Bruin says. “Even among people who initially wanted the vaccine, a surprising share—16%—said they no longer wanted it after they were passed over. Public health officials should keep this dynamic in mind when developing plans in the future.”
The study, published in the Journal of Risk Research, drew from consumer research showing that when people are overlooked during the initial allocation of a product they will lose interest. While COVID-19 vaccines are now widely available in the U.S., certain groups had to wait initially. In countries where supplies are limited, people are still waiting.
Contributing to the discussion about vaccines, Karen Mulligan and Jeffrey Harris authored a Schaeffer Center white paper evaluating the effectiveness of workplace vaccine mandates, finding that they are sound public policy. Furthermore, they argued, the federal government has an important role to play in endorsing these mandates while making sure vulnerable communities are protected.
Leveraging Rapid Antigen Testing for Schools
As we build a new normal, keeping kids safe in schools—while ensuring the best learning environment—is critical. Neeraj Sood led one of the first studies in the country evaluating the use of rapid antigen tests in children.
The tests show promise, especially if schools use serial testing, such as twice a week.
“Serial testing is critical because one-time antigen tests might not identify asymptomatic children at or shortly after the onset of infection,” Sood says. “But serial testing will likely identify these children as they subsequently develop high viral loads and become infectious a few days later.”
Sood presented his results to the California Department of Education as it was evaluating best practices for the state. He also presented at an expert panel for the National Academies of Sciences, Engineering and Medicine.

Neeraj Sood, Director, COVID Initiative.

- “It was the inability to scale the development and deployment of diagnostic tests [that] was really at the root of a lot of our challenges with this coronavirus.”
– Scott Gottlieb, former FDA Commissioner -
U.S. healthcare markets have many inefficiencies, resulting in both overuse and underuse of healthcare. The Schaeffer Center is conducting research to analyze the most appropriate market incentives for motivating individuals and stakeholders to improve the functioning of the healthcare system.

Adding Value to Older Heart Patients’ Lives
Traditional treatments for valvular heart disease—a condition affecting more than 13% of adults age 75 and older—have been open-heart surgery or symptom management. But less invasive options are available, an important development for patients considered too high risk for conventional surgery.
Schaeffer Center researchers evaluated the social value of transcatheter aortic valve replacement (TAVR), finding it has the potential to generate billions in social value. Yet uptake remains low.
“More than half of aortic stenosis patients are still being medically managed instead of receiving TAVR,” Darius Lakdawalla notes. Developing policies and procedures to incentivize TAVR use in appropriate patient populations should be an important priority for Medicare, he says.
Updating Regulation and Reimbursement
Millions of Americans rely on medical devices every day. Yet antiquated systems for regulating and paying for such advances can have serious consequences. For instance, shortages of COVID-19 tests have dramatically hindered the nation’s response to the pandemic.
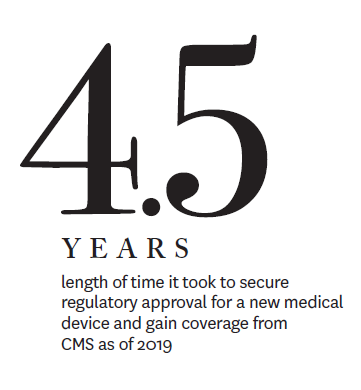
To address these issues, the Richard N. Merkin, MD, Distinguished Speaker Series hosted a talk with Nonresident Senior Fellow and former Director of the Domestic Policy Council Joe Grogan and former Food and Drug Administration (FDA) Commissioner Scott Gottlieb. Erin Trish moderated the conversation, which covered the challenges faced by the FDA and the Centers for Medicare & Medicaid Services (CMS) in ensuring that effective devices can be brought to patients more quickly.
“It was the inability to scale the development and deployment of diagnostic tests [that] was really at the root of a lot of our challenges with this coronavirus,” Gottlieb said. “And it was largely a failure of the ability of the federal government to engage private industry early enough and do a handoff to private-sector medical-device manufacturers and get them into the game at the outset.”
Grogan noted the differences between drugs and devices in terms of regulation and payments. For devices, he noted, it “frequently takes multiple years, through several different bureaucratic agencies at CMS … to prove … that your device or diagnostic is appropriate for the Medicare population. And private industry keys off of Medicare for figuring out what to cover or not.”
New Leadership
Matthew Kahn, provost professor of economics at the USC Dornsife College of Letters, Arts and Sciences, will lead the Healthcare Markets Initiative along with Jakub Hlávka, research assistant professor at the USC Price School of Public Policy. Kahn is a nationally recognized environmental economist focused on urbanization, climate change, and the effects of these issues on health and quality of life.
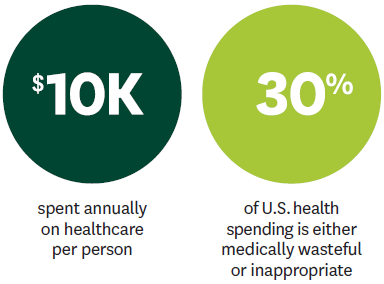
“There is significant waste in the U.S. healthcare system,” Kahn says. “Through the Healthcare Markets Initiative, we will bring together thought leaders to identify solutions that improve health outcomes and efficiency. The future of healthcare in this country depends on new approaches to these tough issues—and leveraging market forces may provide some clear answers.”
Hlávka’s research includes work on innovative payment models for pharmaceuticals, health system reform and the study of inequality. For example, pharmaceuticals are priced uniformly by convention, but many medicines have different levels of effectiveness in different patients. This is one of many market inefficiencies in drug pricing. Analysis by Hlávka, Darius Lakdawalla and Dana Goldman focused on the economics of alternative payment models to uniform pricing and highlighted challenges policymakers, payers and other stakeholders should be aware of as these options are considered.
While implementation faces numerous challenges, including regulatory and data-collection constraints, they predict value-based agreements for pharmaceuticals will be relied on more extensively as solutions to the implementation challenges are identified.

Jakub Hlávka and Matthew Kahn, leaders, Healthcare Markets Initiative.

- How do we expand access, improve patient protections and build a more affordable healthcare market? The USC-Brookings Schaeffer Initiative for Health Policy unites the Schaeffer Center’s data and analytic strengths with Brookings Institution’s economic policy expertise. The initiative is a major resource for rigorous analysis and practical solutions relied upon by policymakers, private-sector leaders and the public.
-
Taking the Sting out of Surprise Billing
Patients have long suffered financial strain from exorbitant surprise medical bills stemming from out-of-network care. Collaborative work under the Schaeffer Initiative has informed numerous pieces of legislation at the state and federal levels to protect consumers from this practice, also known as balance billing.

The most sweeping of these is the federal No Surprises Act, which went into effect January 1, 2022. In addition to making it illegal to bill patients for more than in-network cost sharing for certain services, the legislation establishes an arbitration process to resolve disputes between providers and insurers. Following the bill’s passage, Schaeffer Initiative researchers continued to conduct analyses, examine the best ways to maximize its effectiveness and write recommendations for implementing the new law, many of which were adopted in the administration’s rulemaking.

In a piece for Medpage Today, Loren Adler and Erin Trish noted that most doctors don’t want to send balance bills to unsuspecting patients and that physicians not currently profiting from surprise billing “could see pay increases because of the law’s new out-of-network price support.”
Furthermore, the No Surprises Act will save money overall because it uses median in-network prices to guide payment decisions—a strategy outlined by the Schaeffer Initiative in early research. “The law is a big win for patients, employers and consumers,” Adler and Trish write.
Bringing Expenses Down to Earth
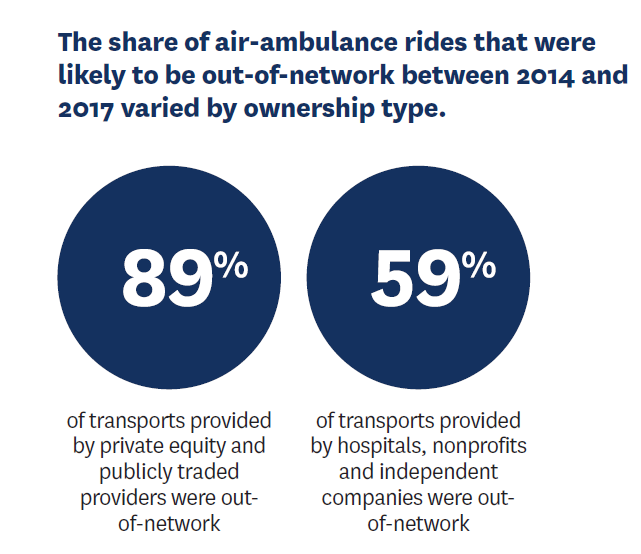
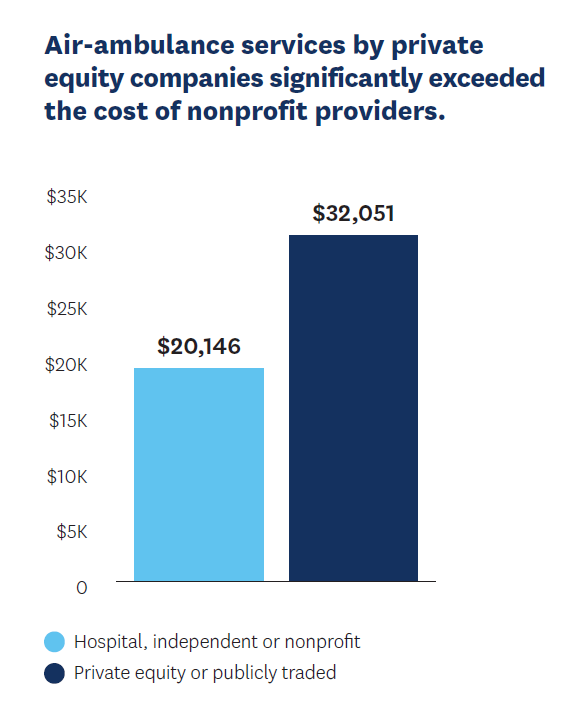
When it comes to emergency services, air ambulances account for some of the highest surprise bills. Lack of competition is a factor as, by 2017, just two private equity firms had gained control of nearly two-thirds of the Medicare market for air-ambulance transport.
Analyzing commercial insurance claims data for 2014–2017, Loren Adler, Erin Trish and colleagues found that emergency medical air transports owned by private equity or publicly traded companies were paid an average of $32,051—5.6 times what Medicare would have paid. This is particularly concerning given that 89% of transports provided by private equity or publicly traded companies during this timeframe were out-of-network.
Fortunately, air-ambulance providers are among those covered by the No Surprises Act, which will protect patients from these surprise bills going forward and should lower prices. However, more can still be done to protect patients and improve the market.
Surprise bills also routinely come from specialty services such as anesthesiology. A study by Adler, Trish, Erin Duffy and Bich Ly sorted through various payment methods for anesthesiologists and certified registered nurse anesthetists, examining 3.59 million commercial and 1.87 million Medicare Advantage claims for common anesthesiology services.
They found that the mean, in-network commercial charge was 659% of the Medicare rate, while the allowed payments were 314% of that rate. The researchers suggest that policymakers “choose out-of-network payment benchmarks prudently” to avoid inflation when using the No Surprises Act as a guide to rein in these expenses. This analysis fills a critical gap in understanding complex payment structures for anesthesiology which have made it hard to reliably compare amounts charged across payers and patient populations.
New Director Named
The USC-Brookings Schaeffer Initiative for Health Policy appointed Richard Frank as its new director in September 2021. He succeeds Paul Ginsburg, who will continue his impactful work for the Center as a senior fellow.
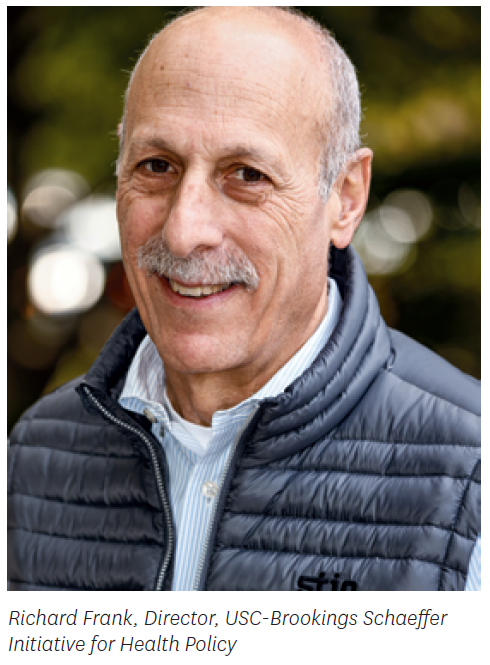
Frank joined the initiative from Harvard Medical School, where he is the Margaret T. Morris Professor of Health Economics Emeritus in the Department of Health Care Policy. His research focuses on the economics of mental health and substance abuse care, financing for long-term care, prescription drug policy, healthcare competition and disability policy.
“The Schaeffer Initiative has had remarkable success informing health policy debates under the leadership of Dr. Ginsburg,” Dana Goldman says. “These include issues such as surprise medical billing, the Affordable Care Act, market competition and drug pricing. Dr. Frank’s record of scholarship and public service makes him the ideal appointment to continue to advance our collaboration.”
From 2014 to 2016, Frank served as assistant secretary for planning and evaluation in the Department of Health and Human Services. His honors include election to the National Academy of Medicine’s Institute of Medicine, the Georgescu-Roegen Prize, the Carl A. Taube Award from the American Public Health Association and the Academy-Health Distinguished Investigator Award.
“With Dr. Ginsburg at the helm, the Schaeffer Initiative has informed policymakers and private-sector leaders about today’s most pressing healthcare issues,” notes Leonard D. Schaeffer, founder of the Schaeffer Center and the USC-Brookings Schaeffer Initiative for Health Policy. “I have no doubt that Dr. Frank will further enhance the initiative’s ability to provide the research and analysis needed to improve health policy at the national level.”
Forward-Looking Reforms
Richard Frank’s leadership of the USC-Brookings Schaeffer Initiative for Health Policy builds on successes achieved under Paul Ginsburg while also adding new priorities—including a focus on mental health. As one of his first activities, Frank and his colleagues submitted a letter to the U.S. Senate Committee on Finance in response to a white paper on mental wellbeing by Senators Michael Bennet (D-Colorado) and John Cornyn (R-Texas).

Frank and his colleagues recommend aligning Medicaid, block grants, state and local funds, and private insurance for mental health services, as well as building on existing payment mechanisms in public insurance programs to increase accountability. Doing more, Frank and longtime colleague Sherry Glied say, “requires policymakers to think creatively about the use of resources—workforce and technology—combine operating funds with infrastructure investments, and demand much more accountability from all providers and funders in the system.”
In a separate piece, Frank and Glied discussed the cost of mental illness in the workplace and the need for businesses to recognize the reality of mental health symptoms and allow for flexibility and accommodation at work. You can do this, they write, and still preserve productivity.

Prescription drug pricing reform continues to hold policymakers’ and the public’s attention. Loren Adler and Paul Ginsburg developed a framework for policymakers evaluating the wide range of proposals, noting the need for awareness of the trade-offs inherent in various policy options. One such trade-off is the balance between innovation and access. This is especially true in oncology, where accelerated approval of new drugs has the potential to improve cancer outcomes, but the cost is high and the value uncertain.
Frank proposed a model, published in JAMA, that would allow payers to only pay for cancer drugs that work. This would incentivize innovation while ensuring money spent on new therapies is well-used. In a piece published in the New England Journal of Medicine, Frank and colleagues elaborated on the trade-off between future innovation and regulating drug pricing.
“These challenges are created in part by our system’s failure to consistently establish prices that reflect treatments’ clinical and economic value,” they write.

Building Back Better Savings?
Among other initiatives, President Biden’s Build Back Better (BBB) act aims to expand Medicaid and Medicare by increasing subsidized marketplace coverage for the uninsured—especially in those states that have chosen not to expand Medicaid—as well as reforming prescription pricing.
Matthew Fiedler explored this proposal’s financial implications for hospitals. He estimated that the margins for hospitals in the 12 states that have not expanded Medicaid would improve by $11.9 billion if all related BBB proposals were put into effect, because they would be reimbursed for at least some services that currently go unpaid. However, BBB includes provisions to “claw back” some of this windfall through restrictions in other areas. By comparison, if Medicaid were implemented in these states, Fiedler calculated those hospitals would see $3.6 billion instead.
Fiedler also analyzed BBB prospects for adding hearing, vision and dental coverage to Medicare during congressional reconciliation and explored ways policymakers could cut the costs of adding this coverage without reducing its generosity.
Reinforcing the Affordable Care Act
Signed into law over a decade ago, the Affordable Care Act (ACA) expanded access to healthcare and insurance coverage to millions of people. Experts with the Schaeffer Initiative continue to analyze the effects of this complex legislation and offer evidence-based guidance aimed at improving the system’s functioning.
At least 2.2 million low-income people living in the 14 states that have not expanded Medicaid are still unable to receive coverage from either traditional Medicaid or the individual marketplace. Richard Frank and Sherry Glied evaluated the various options policymakers could use to solve this critical gap in coverage in an issue brief published by Commonwealth Fund. The piece has been a resource for policymakers as they discuss proposals.
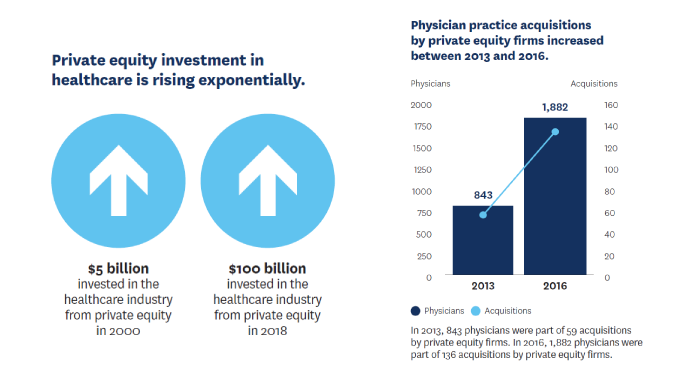
Evaluating Private Equity Investment’s Impact on Markets
The growing number of physician-practice acquisitions by private equity has prompted concerns about potential effects on quality, prices and access to care.
Paul Ginsburg, Loren Adler, Erin Duffy and Samuel Valdez worked with colleagues to develop strategies for reducing the hazards of acquisitions, including closing payment loopholes that raise costs for consumers and taxpayers as well as strengthening antitrust and fraud enforcement.
However, since private equity also carries benefits such as capital infusions that could aid patient care, the authors urge policymakers to balance the advantages and disadvantages when considering such policies.

- The Schaeffer Center’s data core and microsimulation teams leverage the information and tools necessary to help answer significant questions in health policy with evidence-based solutions.
-
Data Core
The data core works to improve the quality and productivity of research through providing organized data resources, training and staff expertise. Including programmers, statisticians, analysts and a data resource administrator, the team has proficiency in the methods and programming necessary to rigorously analyze big data. Schaeffer Center fellows and students rely on this team for support on a range of projects.
Data Library and Data Security
The Schaeffer Center’s data library includes survey data, public and private claims, contextual data and electronic health network data feeds. The data core is a pioneering information resource and computing environment that meets exacting standards of excellence in data security through a mix of security measures—from an air-gapped workstation to state-of-the-art, Health Insurance Portability and Accountability Act (HIPAA)-compliant systems that include 24/7 monitoring to ensure resources are protected.
Health Policy Microsimulation
For more than a decade, the Schaeffer Center has been at the forefront of developing pioneering economic demographic microsimulation tools to effectively model future trends in health and longevity and answer salient questions in health policy. The centerpiece effort is the Future Elderly Model (FEM), which projects a rich set of health and economic outcomes for the U.S. population age 50 and older. The FEM was originally designed to answer questions about the long-term economic viability of the Social Security and Medicare programs. Schaeffer Center researchers have since used the FEM to explore an increasingly wide variety of policy questions, ranging from the fiscal future of the U.S. to the role that biomedical innovation can play in health outcomes.
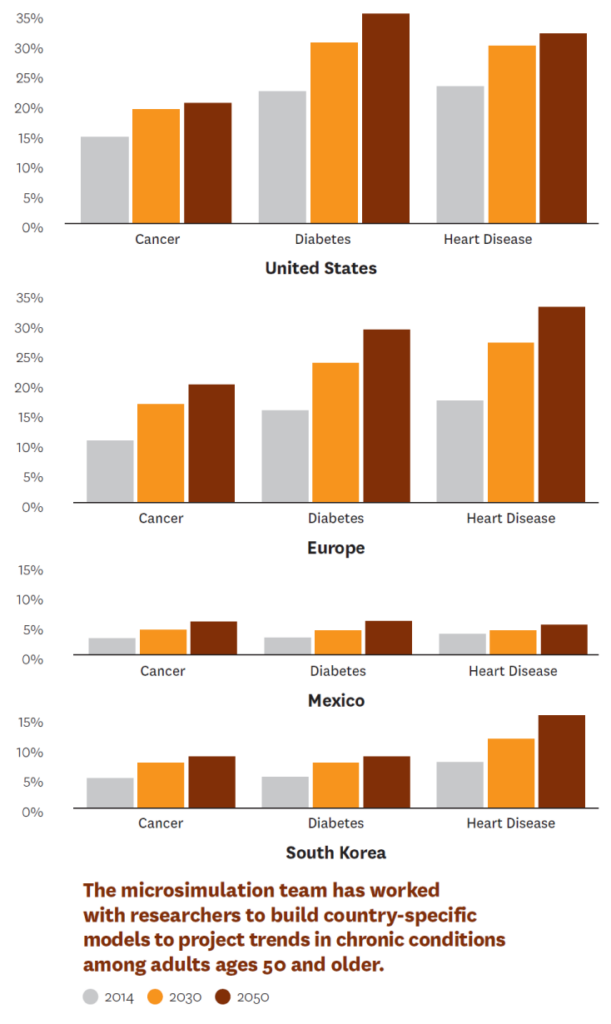
The microsimulation team is building a network of collaborators to develop country-level, FEM-based models in nations around the world. This effort will allow researchers to compare demographic, health and economic trends on a global scale.
Researchers recently used the FEM to forecast long-term trends in disease dynamics in 15 countries. Focusing on investigating the consequences of policy and behavioral factors in healthy aging, including trends in chronic disease, education and behavioral factors like smoking, the researchers produced forecasting models that can be used by policymakers and stakeholders. Researchers involved in the project include two winners of the Nobel Prize in Economics, Daniel McFadden and James Heckman. This work resulted in eight papers published as part of a special issue of Health Economics.
Models have also gone local, with simulations conducted for California and Los Angeles County to help policymakers at the state and county levels understand trends and the impact of policy decisions.
Ultimately, the goal is to offer a tool to help policymakers weigh the pros and cons of potential policies, using actual evidence about impact when deciding where to put resources. Findings using the FEM and the related Future Adult Model have been published in top journals and cited or commissioned by government agencies, the White House, the National Academy of Sciences and private organizations interested in aging policy.
Data Partnerships and Collaborations
In addition to being a resource for Schaeffer Center researchers, the data core and microsimulation teams partner with local, state, federal and international collaborators to develop data projects and models. Key collaborators include the National Academies of Sciences, Engineering and Medicine, and the Los Angeles County Department of Public Health.

Bryan Tysinger, Director, Health Policy Microsimulation.

You must be logged in to post a comment.