Day 1: COVID-19 Changed Patient Preferences For When, Where and How to Receive Care. Will These Trends Prove Durable Post-Pandemic, and What Do They Mean for Long-Term Health and Costs?
The COVID-19 pandemic has changed the way Americans make their healthcare decisions. Periods of high and rising cases have quickly pushed health systems past capacity, forcing providers to cancel non-COVID procedures. Furthermore, patients now recognize that physician visits and procedures that once seemed routine and mundane now carry the risk of exposure to a highly transmissible and dangerous disease. According to the CDC, 41% of U.S. adults have skipped care during the pandemic. We have yet to fully understand the long-term health and cost implications of this delayed or foregone care.
Join the Schaeffer Center for a two-part series on the pandemic’s effects on the kind of care patients are seeking, what they value and prefer, and the need for healthcare systems, payers, and policymakers to meet this challenge in an equitable way. Day one will focus on how patient preferences have changed and what we know about whether these trends will prove durable post-pandemic.
This is the first part of a two-part webinar. View Day 2 here.
- Event Date
- Tuesday, March 23, 2021
1:00 PM - 2:00 PM Pacific - Location
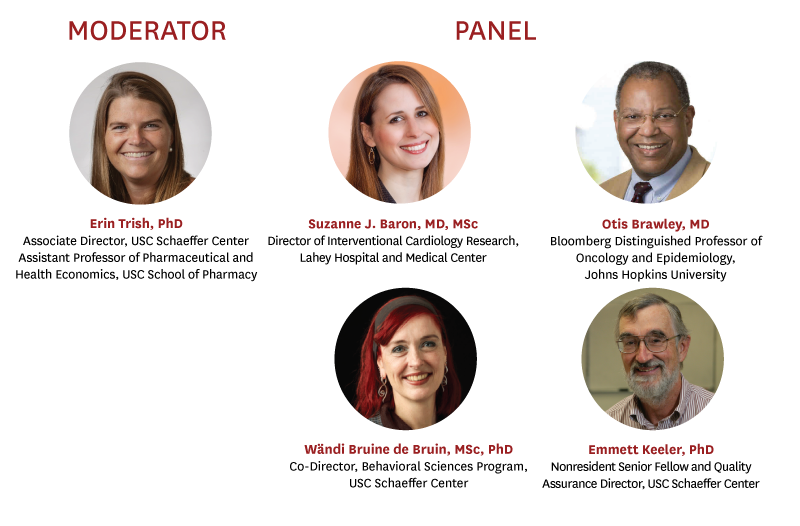
Erin Trish, PhD (Moderator) -- Featured Presentation: Changing Care Patterns since COVID-19
Associate Director, USC Schaeffer Center
Assistant Professor of Pharmaceutical and Health Economics, USC School of Pharmacy
Erin Trish is associate director of the USC Schaeffer Center and an assistant professor of pharmaceutical and health economics at the USC School of Pharmacy. In addition, she is a nonresident fellow in Economic Studies at the Brookings Institution and a scholar with the USC-Brookings Schaeffer Initiative for Health Policy.
Her research focuses on the intersection of public policy and health care markets, with recent projects focused on surprise medical bills, prescription drug spending, health care market concentration, and health care reform. Her research has been funded by grants from the Robert Wood Johnson Foundation and the Laura and John Arnold Foundation and published in leading health policy, health economics, and medical journals. She has testified in the California State Assembly and presented her research at numerous federal agencies, including the Congressional Budget Office, Federal Trade Commission, Office of the Assistant Secretary for Planning and Evaluation, and the Center for Consumer Information and Insurance Oversight. In 2018 she received the Seema Sonnad Emerging Leader in Managed Care Research Award.
Trish completed a postdoctoral fellowship at the USC Schaeffer Center and the Fielding School of Public Health at the University of California, Los Angeles. She received her PhD in Health Policy and Economics from the Johns Hopkins Bloomberg School of Public Health and her BS in Biomedical Engineering from Johns Hopkins University.
Suzanne J. Baron, MD, MSc
Director of Interventional Cardiology Research, Lahey Hospital and Medical Center
Suzanne J. Baron, MD, MScis the Director of Interventional Cardiology Research at Lahey Hospital and Medical Center in Burlington, Massachusetts, where she practices as an interventional cardiologist, specializing in structural heart interventions. She has an interest in value-based care and her research focuses on evaluating the effects of novel cardiovascular devices on patient-reported outcomes and health care costs.
Otis W. Brawley, MD
Bloomberg Distinguished Professor of Oncology and Epidemiology, Johns Hopkins University
Otis W. Brawley, MD, MACP, FASCO, FACE is the Bloomberg Distinguished Professor of Oncology and Epidemiology at Johns Hopkins University. He is a board certified medical oncologist and an epidemiologist. He is an authority on cancer screening and prevention and leads a broad research effort of cancer health disparities at the Johns Hopkins School of Medicine, Bloomberg School of Public Health and the Sidney Kimmel Comprehensive Cancer Center, focusing on how to close racial, economic, and social disparities in the prevention, detection, and treatment of cancer. From 2007 to 2018, Brawley was Chief Medical and Scientific Officer of the American Cancer Society. He is recipient of the U.S. Public Health Service (PHS) Meritorious Service Medal, the Department of Defense Distinguished Service Award and the 2019 American Medical Association Distinguished Service Award. He is also a member of the National Academy of Medicine.
Wändi Bruine de Bruin, MSc, PhD
Co-Director, Behavioral Sciences Program, USC Schaeffer Center
Provost Professor of Public Policy, Psychology, and Behavioral Science, USC Price School of Public Policy
Behavioral Scientist, USC Center for Economic and Social Research
Wändi Bruine de Bruin, MSc, PhD is the Provost Professor of Public Policy, Psychology, and Behavioral Science at the USC Price School of Public Policy. Bruine de Bruin’s research aims to understand and inform how, across the life span, people make decisions about their health, their well-being, and their environmental impacts. She has published over 100 peer-reviewed papers on these topics, in journals targeting psychology, public policy, health, and environmental science. She is a member of the editorial boards of the Journal of Experimental Psychology:Applied, the Journal of Behavioral Decision Making, Decision, Medical Decision Making, the Journal of Risk Research, and Psychology and Aging. Her research on age differences in decision making was recently covered by Psychology Today and the BBC World’s Why Factor. She has served on expert panels for the National Academy of Sciences on Communicating Science Effectively and for the Council of the Canadian Academies on Health Product Risk Communication.
Emmett Keeler, PhD
Nonresident Senior Fellow and Quality Assurance Director, USC Schaeffer Center
Professor, Pardee RAND Graduate School
Emmett B. Keeler is a professor in the Pardee RAND Graduate School and an adjunct professor at the UCLA Public Health School, where he has taught cost-effectiveness analysis and decision analysis in medicine and public health for many years.
In 1997, he set up the quality assurance procedures for the RAND Health Program reports, and led the quality assurance office until 2005. He analyzed health outcomes and episodes of spending for the RAND Health Insurance Experiment. He led the multi-site Improving Chronic Illness Care Evaluation and the Management of Childbirth PORT.
His recent work has involved the costs of lung cancer screening and policies to promote cost-lowering new technologies. He was the Academy Health Distinguished Investigator in 2003.
An elected member of the Institute of Medicine (IOM), he has participated in IOM committees on the scientific basis for the polygraph, on incorporating uncertainty into environmental decisions, the economic costs of uninsurance, the use of health measures in regulatory analysis, national health accounts and what to do about geographic variation in healthcare spending. He earned his PhD in mathematics from Harvard University.