A new USC Schaeffer Center study shows the return on investing in improving educational attainment for those diagnosed with serious mental illness by age twenty-five, projecting positive impacts on health and economic outcomes.
Serious mental illness (SMI) imposes devastating costs to a person’s life, impacting healthcare costs, education, work, and life expectancy. The individual economic burden of SMI is high, comparable to cancer and diabetes, and further exacerbated by the relatively young age of onset.
While there is acceptance that early intervention has lifetime benefits for people with serious mental illness, there has been little evidence to support this assumption, in part because many studies do not follow individuals for their entire life and thus cannot capture the lifetime benefits. A new study, published in the April 2019 edition of Health Affairs, uses a microsimulation model to estimate the lifetime burden of SMI for individuals diagnosed before the age of twenty-five.
The researchers estimate the lifetime burden of SMI to be $1.85 million per patient. They also estimate that an intervention that successfully improved educational attainment for patients with SMI would result in a reduced burden of over $73,000 per patient.
“Our findings point to the importance of policies that promote early identification and access to appropriate services in support of individuals with SMI,” said Seth Seabury, first author on the paper and an associate professor at the USC School of Pharmacy and the Schaeffer Center for Health Policy & Economics. “Left untreated, SMI can have lasting negative effects on all parts of a person’s life. Early diagnosis and intervention is key to getting people onto a better path and can have lifelong benefits.”
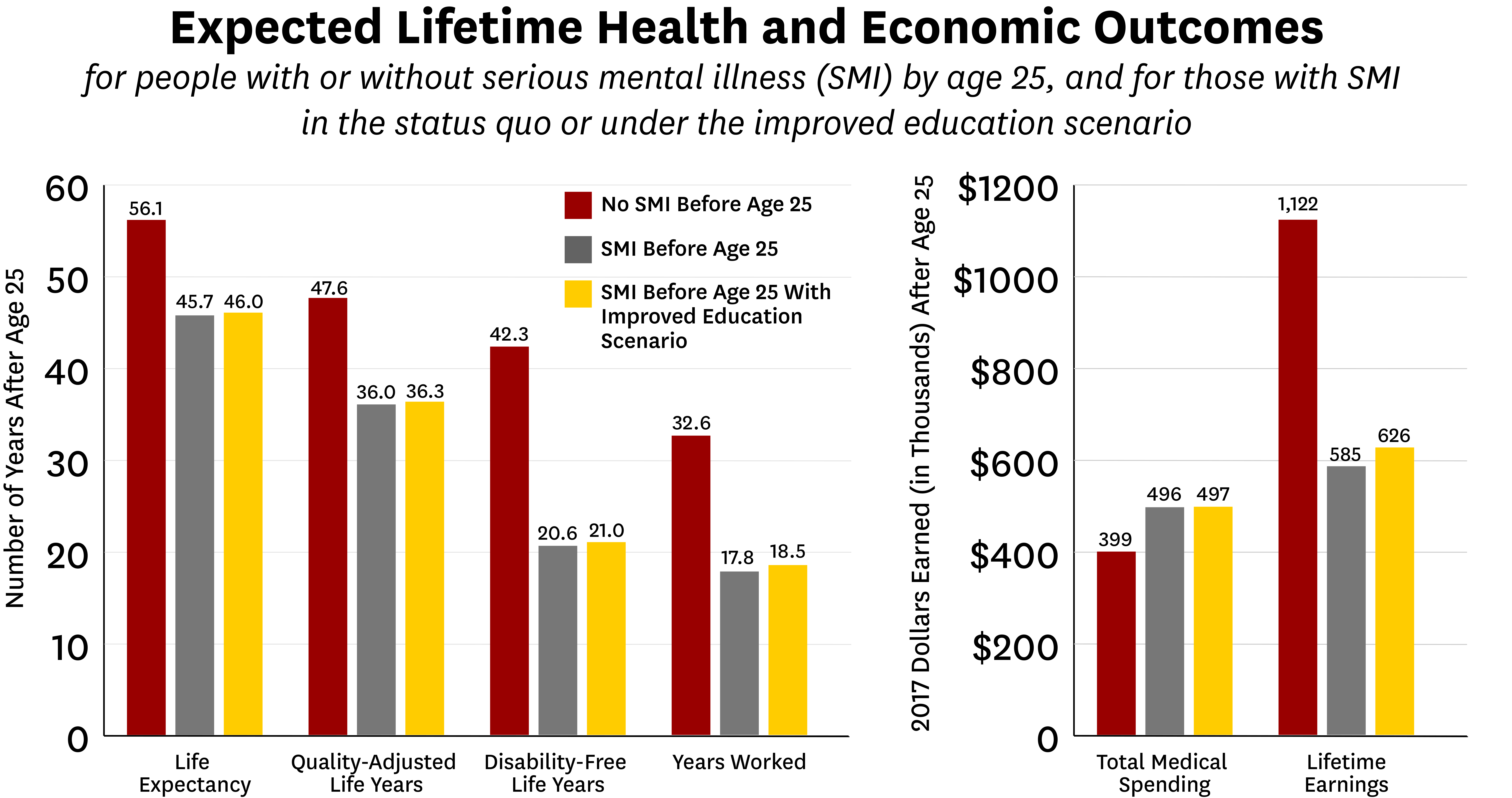
Serious mental illness collectively includes psychoses, major depressive disorder, and bipolar disorder. While previous studies have shown the positive impacts of early identification, diagnosis and treatment on quality of life, they do not assess the benefits of these interventions across an individual’s life span. This study provides new data on the lifetime benefits of improving educational outcomes for people who experience SMI early in life. Using the Schaeffer Center Future Adult Model, the researchers simulated the lifetime outcomes of people with and without SMI by the age of twenty-five.
Results of the simulations show SMI significantly worsens lifetime health outcomes, raises medical costs, and reduces economic outcomes. People with SMI by age twenty-five had an average life expectancy loss of over ten years and lifetime earnings $537,000 less than those without SMI by age twenty-five.
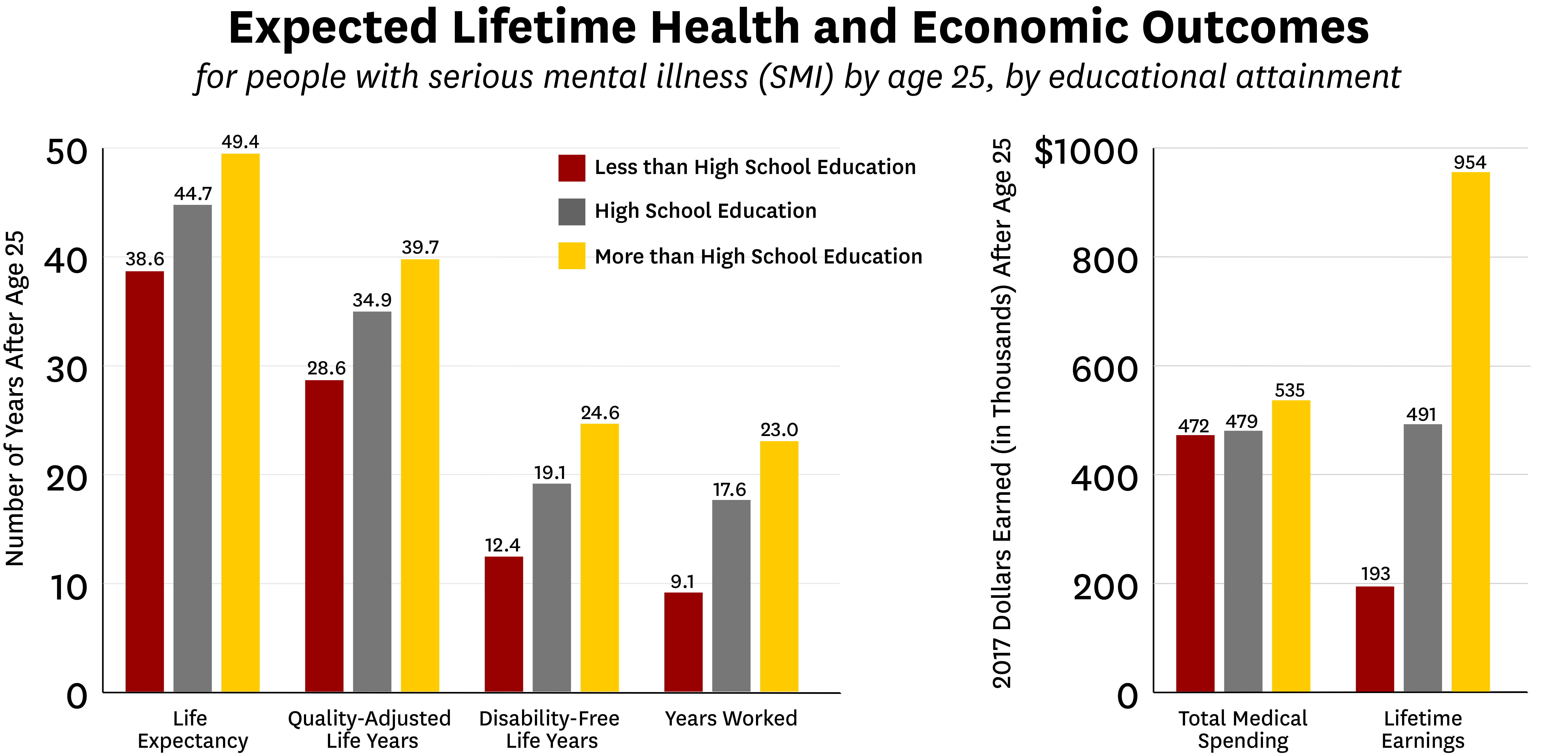
“Educational attainment mitigates some of these negative effects,” said Sarah Axeen, an author on the study and assistant professor at the Keck School of Medicine of USC and the USC Schaeffer Center. “Across all outcomes we measured, people with SMI are worse off on average than their counterparts, regardless of their level of education. But, higher educational attainment lessens these burdens. Most strikingly, we find that those with more than a high-school education average $954,000 in lifetime earnings compared to those with less than a high-school education who average $192,900.”
The study results show that the economic burden of each new cohort of SMI patient experiences nearly a quarter of a trillion dollars in economic burden, and the simulated improvement in educational attainment would produce a reduction of over $8.9 billion. While such an intervention might be costly, the authors estimate a two-year educational intervention would produce a two-to-one return on investment compared to the cost of the intervention. The authors note that widely implementing the interventions necessary to spark increased educational attainment would require an investment in increasing behavioral health services.
Other authors of the study include Gwyn Pauley, Bryan Tysinger, Danielle Schlosser, John B. Hernandez, Hanke Heun-Johnson, Henu Zhao, and Dana P. Goldman. The research was supported by the National Institute on Aging (grant P30AG024968), and through unrestricted grants to the Leonard D. Schaeffer Center for Health Policy & Economics from Verily Life Sciences and Alkermes.
###
ABOUT THE LEONARD D. SCHAEFFER CENTER FOR HEALTH POLICY & ECONOMICS
The mission of the Leonard D. Schaeffer Center for Health Policy & Economics is to measurably improve value in health through evidence-based policy solutions, research and educational excellence, and private and public sector engagement. A unique collaboration between the Sol Price School of Public Policy at the University of Southern California (USC) and the USC School of Pharmacy, the Center brings together health policy experts, pharmacoeconomics researchers and affiliated scholars from across USC and other institutions. The Center’s work aims to improve the performance of health care markets, increase value in health care delivery, improve health and reduce disparities, and foster better pharmaceutical policy and regulation.

You must be logged in to post a comment.