Editor’s note: This perspective is a summary of a JAMA Health Forum Viewpoint published on August 26, 2022.
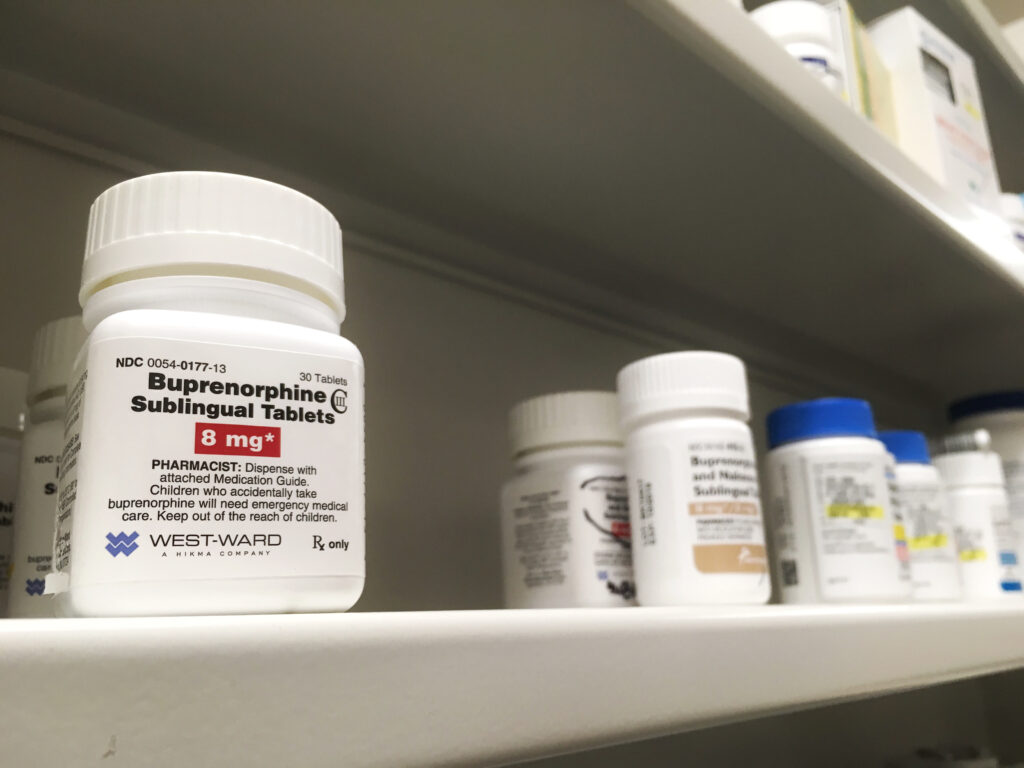
Buprenorphine is currently the only scheduled medication approved for the treatment of opioid use disorder (OUD) that can be prescribed in primary care settings and dispensed at retail pharmacies. Despite buprenorphine’s potential to increase access to OUD treatment, nearly 80% of people with OUD still go without treatment, and racial disparities persist in OUD treatment and recovery in the US. Policy efforts to reduce these gaps have largely ignored the role of restrictive pharmacy regulations.
For a Viewpoint published in JAMA Health Forum, Dima M. Qato and colleagues discuss regulations that may create dispensing barriers at retail pharmacies and propose several policy solutions.
Policy efforts attempting to reduce treatment barriers have focused on prescribing regulations—including expanding who can prescribe buprenorphine, and how much they can prescribe, lifting requirements for in-person visits for new patients and expanding e-prescribing. But they have not considered the role of federal and state pharmacy regulations after buprenorphine is prescribed.
Policy efforts attempting to reduce treatment barriers have focused on prescribing regulations—including expanding who can prescribe buprenorphine, and how much they can prescribe, lifting requirements for in-person visits for new patients and expanding e-prescribing. But they have not considered the role of federal and state pharmacy regulations after buprenorphine is prescribed.
Dima Qato, Senior, USC Schaeffer Center
Suppliers, pharmacies and pharmacists must comply with existing pharmacy regulations governed by the Controlled Substances Act (CSA) to distribute or dispense buprenorphine because it is a Schedule-III controlled substance.
Sign up for Schaeffer Center news
Qato and colleagues pinpoint three important dispensing barriers:
- Suppliers often delay or suspend buprenorphine shipments because growing demand for buprenorphine prescriptions— which should be expected— can lead to pharmacies being flagged as “suspicious.
- Pharmacies frequency do not stock buprenorphine because of worries that suspicious orders or activity may be reported to the DEA.
- Even when the drug is in stock, pharmacists may refuse to dispense for fear of violating the CSA and their corresponding responsibility or legal duty ensure the validity of prescriptions for controlled substances.
The authors propose several policy solutions to address dispensing barriers and expand access to buprenorphine treatment. The rationale for these policy changes is that buprenorphine is subject to existing pharmacy regulations initially designed to prevent the diversion, misuse and abuse of controlled substances, especially opioids, and were not intended for scheduled medications for OUD like buprenorphine.
The solutions include:
- Exempting buprenorphine from the CSA and DEA-dispensing regulations when prescribed for treatment of OUD.
- Changing state and federal laws to protect suppliers, pharmacies and pharmacists from any liability associated with buprenorphine distribution and dispensing.
- Developing corresponding responsibility and red-flag guidelines specific for buprenorphine.
Qato add that, although the Drug Addiction Treatment Act of 2000 amended the CSA to expand access to OUD treatment to primary care, the CSA has not been modified to ensure dispensing regulations intended to prevent opioid diversion do not also restrict access to buprenorphine at retail pharmacies.
Failing to recognize and address dispensing barriers, risks undermining the impact of efforts aimed solely at expanding buprenorphine prescribing on OUD treatment and recovery and worsening racial disparities in buprenorphine treatment in the U.S.
Dima Qato, Senior Fellow, USC Schaeffer Center
In addition to Qato, authors of the piece include Jonathan Watanabe of UC Irvine School of Pharmacy & Pharmaceutical Sciences and Kelly Clark of Addiction Crisis Solutions. Read the full viewpoint at JAMA Health Forum.
Related Work