What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To sign up to receive the Essential Scan straight to your inbox, sign up here.
Strict Prescription Drug Monitoring Programs Effective Along Measures of Opioid Misuse
Study by: Thomas C. Buchmueller and Colleen Carey
In an attempt to curb opioid abuse, many states have implemented Prescription Drug Monitoring Programs (PDMPs) with various degrees of provider access and use requirements. PDMPs collect data on controlled substance prescriptions to facilitate detection of suspicious prescribing and use patterns. In a new study, researchers used a difference-in-difference model to assess the effectiveness of PDMPs on opioid prescription levels among Medicare beneficiaries. They found states with the strongest laws, which cover all ingredients, settings of care, and do not require providers to be suspicious, had the largest effects on measures of misuse whereas PDMPs with voluntary use provisions have no effect. For example, in states with “must access” provisions, the percentage of Medicare Part D enrollees who obtain prescriptions from five or more prescribers fell by 8 percent and the percentage of enrollees who obtain prescriptions from five or more pharmacies fell by 15 percent compared to states without such provisions. However, the researchers found no statistically significant effect on opioid poisoning incidents. Full study here.
Employers Offered Less Generous Health Plans During the Great Recession
Study by: Kanghyock Koh

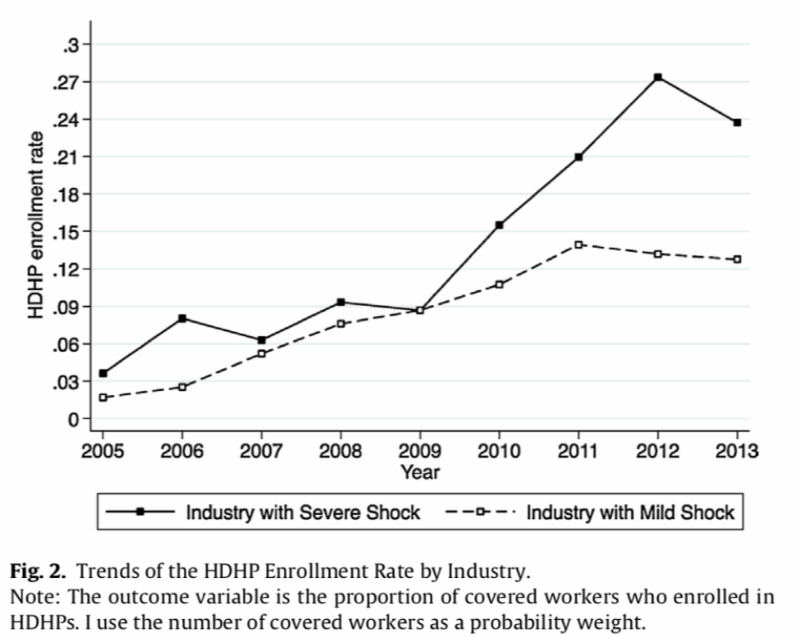
“Offering high-deductible plans and increasing what employees pay for low-deductible plans may be the area where employers have the most flexibility to cope with cyclical shocks.”
-Paul Ginsburg, PhD, Director, USC-Brookings Schaeffer Initiative for Health Policy
During economic downturns, employers face substantial pressure to reduce compensation for their workers in order to cut costs. However, since employers can only lower wages so much before their employees are forced to seek work elsewhere, they can attempt to save money in a subtler way by decreasing the generosity of the employer sponsored health benefits offered to employees. A researcher used the Employer Health Benefits Survey (EHBS) to show that employers experiencing severe recession shocks during the Great Recession employed this tactic and were 4.1 percent more likely to only offer high deductible health plans (HDHPs) and increased the price of their low deductible health plans (LDHPs) relative to their HDHPs by $354 per year on average. According to the study, the increase in HDHP enrollment rates was not driven by more employees choosing to enroll in HDHPs to save money due to the recession. The author suggests that the Affordable Care Act’s employer mandate, which increases the cost of offering health benefits to employees, could lead employers to continue to cut costs by shifting more employees into HDHPs. Full study here.
Study by: Mark Duggan, Jonathan Gruber, and Boris Vabson
Although Medicare has become increasingly reliant on private insurance companies as a result of the implementation of the Medicare Advantage (MA) and Part D programs, there is limited evidence of any relative efficiency advantages gained through the use of MA plans. A new study leverages hospital discharge data from New York state to evaluate changes in care demanded after patients were forced to move from MA to traditional fee-for-service (FFS) plans following their MA plan’s complete exit from their county of residence between 1998 and 2003. The researchers found Medicare beneficiaries who were originally in MA plans increased hospital utilization by 60 percent, total hospital days by 48 percent, and total number of hospitals procedures by 33 percent, following a move back to FFS. The increase appeared to be persistent over the three years following plan exit, suggesting this wasn’t due simply to pent up demand. However, the authors find this increase was not associated with higher quality of care or a reduction in mortality. This suggests MA plans may be more efficient in providing care than the traditional FFS program– an important finding for policymakers to consider as the fiscal sustainability of Medicare is debated. Full study here.
Subsidization of Long-Term Care Reduces Hospital Admissions and Utilization
Study by: Joan Costa-Font, Sergi Jimenez Martin, and Cristina Vilaplana
Policymakers in the United States have long attempted to reduce health spending by lowering rates of hospital readmission. Reducing readmission rates has been very difficult, though, because the American population is aging rapidly and elderly patients are more prone to readmission. In 2007, Spain, which faced similar demographic shifts, extended its public subsidization of long-term care services (LTCS) which created universal access to previously means-tested LTCS. However, in 2012 the program was rolled back due to austerity cuts, providing a unique research opportunity. Researchers used data from the Survey of Health, Ageing, and Retirement in Europe 2004-2013 to test the Spanish program’s effect on preventing hospital admissions, as well as early discharges that reduced the length of stay for an individual. Using a difference-in-difference model, the researchers found evidence of a reduction in hospital admissions and utilization after the reform — accounting for an 11.17 percent reduction in hospital costs, with 4.95 percent due to a reduction in admissions and 6.22 percent due to a reduction in the length of stay. The program also led to an increase in outpatient care as well as a reduction in the prevalence of mental health symptoms and loneliness. But the study did not examine whether the savings in hospitalization were sufficient to offset the higher spending for LTCA. Full study here.
The Essential Scan is produced by the USC-Brookings Schaeffer Initiative for Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics.
You must be logged in to post a comment.